表2B-1. feedint tubeの幽門前後構造化抄録
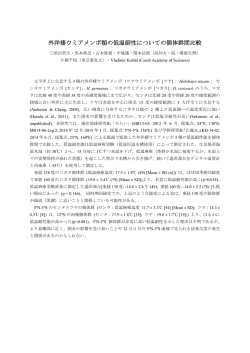
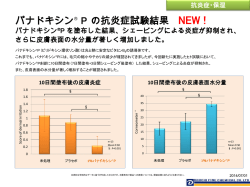
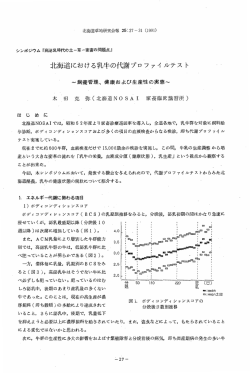
表2B-1. feedint tubeの幽門前後構造化抄録 Title Author reference Nutritional outcome and pneumonia in critical care patients randomized to gastric versus jejunal tube feedings. The Critical Care Montecalvo MA, Crit Care Med Research Steger KA, Farber 1992, 20:1377Team. HW, et al. 1387. Duodenal versus gastric feeding in ventilated blunt trauma patients: a randomized controlled Kortbeek JB, trial. Haigh PI, Doig C. 患者背景 比較群 MICU/SICU (n =SB(n=19) 38) ICU死亡率 肺炎発症率 ICU在室日数 在院日数 平均±SD 人工呼吸期間mean 栄養の結果 ± SD 平均±SD エネルギー充足率 5/19 (26%) 4/19 (21%) 11.7± 8.2 人工呼吸患 者。 APACHE2=23( mean) N=38、 2 ICUs Gastric(n=19) 5/19 (26%) 6/19 (32%) 12.3 ± 10.8 11.4 ± 10.8 46.9% ± 25.9% 中央値(範囲) 中央値(範囲) 中央値(範囲) 目標到達時間 Trauma 1999, 46:992996, discussion 996-998. 外傷 (n = 80) SB(n=37) 4/37 (11%) 外傷 Injury Severity Score16以上 人工呼吸が2 日を越える N=80、 2 ICUsAPACHE 2=18(mean) Gastric(n=43) 3/43 (7%) Prospective, randomized, controlled trial to determine the effect of early enhanced enteral nutrition on clinical outcome in mechanically ventilated patients Taylor SJ, Fettes Crit Care Med suffering head SB, Jewkes C,et 1999;27:2525injury. al. 31 SB(n=41) 5/41 (12%)at 6 mo 10.2 ± 7.1 合併症 GI bleeding 7/19 (37%) Diarrhea 12/19 (63%) Vomiting 3/19 (16%) GI bleeding 6/19 (32%) Diarrhea 9/19 (47%) Vomiting 3/19 (16%) 61.0% ± 17.0% 10 (3-24) 30 (6-47) 9 d (2-13 d) 34.0 ± 7.1 h 18/43 (42%) 7 (3-32) 25 (9-88) 5 d (3-15 d) 43.8 ± 22.6 h エネルギー充足率 窒素投与充足率 59.20% 68.70% 36.80% 37.90% 頭部外傷で10 歳を越える N=82 Gastric(n=41) 6/41 (15%)at 6 mo 26/41 (63%) NR For Puclic Comment 表2B-1. 1ページ C.Random: not sure ITT: no Blinding: no C.Random: yes ITT: yes Blinding: no 10/37 (27%) 18/41 (44%) 統計の条件 37 % major complications 61 % had better neurological outcome at 3 months 61 % major complications 39 % had better neurological outcome at 3months C.Random: not sure ITT: yes Blinding: no 不採用の理由 平均±SD The incidence of ventilatorassociated pneumonia and success in nutrient delivery with gastric versus small intestinal feeding: a Crit Care Med randomized Kearns PJ, Chin 2000, 28:1742clinical trial. D, Mueller L, et al. 1746. Early versus delayed feeding with an immuneenhancing diet in patients with severe Minard G1, head Kudsk KA, injuries. Melton S, etal. MICU (n = 44) SB(n=21) 5/21 (24%) MICU 人工呼吸を必 要としている 症例 APACHE 2=21(mean) N=44 Gastric(n=23) 6/23 (26%) 4/21 (19%) 17 ± 2 39 ± 10 69% ± 7% 18 ±1 3/23 (13%) 16 ± 2 43 ± 11 平均±SD 平均±SD 47% ± 7% 12 ± 2 5日以上目標の 50%以上栄養投 目標到達時間 与出来た症例 (h) 0.7 ± 0.1 0.4 ± 0.1 平均エネル ギー投与量 (kcal/day) 下痢 3日 C.Random: not sure ITT: yes Blinding: no 下痢 2日 JPEN J Parenter Enteral Nutr. 2000 ;24:1459. SB(n=12) 外傷 GCS 3-10 N=27 Gastric feeding with erythromycin is equivalent to transpyloric feeding in the Boivin MA, Levy critically ill. H: 平均±SD 平均エネルギー 投与量 平均蛋白投与 エネルギー充足率 (kcal/day) 量g/kg/day) 1/12 (8%) Gastric(n=15)4/15 (27%) Crit Care Med MICU/SICU/n 2001, 29:1916- euro ICU (n = 1919. 80) SB(n=40) 18/39 (46%) 重症患者 APACHE2=16. 5(mean) N=80 Gastric(n=40) 18/39 (46%) 6/12 (50%) 18.5 ± 8.8 30 ± 14.7 7/15 (47%) 11.3 ± 6.1 21.3 ± 14.7 10.4 ± 6.1 d7/15 (47%) 目標到達時間 NR 15.1 ± 7.5 d10/12 (83%) 33 h 32 h For Puclic Comment 表2B-1. 2ページ 33 ± 15 1509 ± 45 C.Random: not sure 84 ± 41 1174 ± 425 ITT: no Bliinding:Yes C.Random: not sure ITT: no Blinding: no エネルギー充足率 Equal aspiration rates in gastrically and transpyloricall Esparza J, Boivin y fed critically MA, Hartshorne ill patients. MF,et al. Intensive Care Med 2001, 27:660664. Gastric versus duodenal feeding in patients with J Neurosci neurological Nurs 2001, disease: a Day L, Stotts NA, 33:148-149, pilot study. Frankfurt A, et al. 155-159. MICU (n = 54) SB(n=27) 10/27 (37%) MICU MV = 98% APACHE =16(mean) N=54 Gastric(n=27) 11/27 (41%) SB(n=13) NR Neurological ICU 72時間 以上栄養療法 が必要と判断 された症例 APACHE =48(mean) N=24 Gastric(n=11) NR Effect of postpyloric feeding on gastroesophag eal regurgitation and pulmonary microaspiratio n: results of a randomized controlled trial. Heyland DK, Drover JW, MacDonald S, et al. Crit Care Med 2001, 29:14951501 Adult ICU patients expected to remain mechanically ventilated for > 72 hours Mean age: 59 years Male: 58% Mean APACHE II score: 22 ND (n = 12) NG (n = 21) NR C.Random: not sure ITT: yes Blinding: no 66.00% 64.00% 栄養チューブ入れ替え 0/14 (0%) 2/11 (18%) NR NR NR 下痢 7/14 (50) 16 per group 9 per group 誤嚥 嘔吐 4/12(33%) 11/21(52.4%) 11/12(92%) 17/21(83%) For Puclic Comment 表2B-1. 3ページ 下痢 5/11 (45) マイクロアスピレーション 食道胃逆流 7.50% 3.90% 39.80% 24.90% C.Random: not sure ITT: yes Blinding: no 平均±SD Randomized comparison of nasojejunal and nasogastric feeding in Davies AR, Crit Care Med critically ill Froomes PR, 2002, patients. French CJ, et al. 30:586-590. MICU/SICU (n =SB(n=34) 73) 4/34 (12%) 2/31 (6%) 13.9 ± 1.8 目標投与量到達時間 NR 消化管出血 3/31 (10%) 下痢 4/31 (13%) 23.2 ± 3.9 h C.Random: not sure ITT: no Blinding no 成人重症症例 MV=90%; APACHE2=20( mean N=73 Gastric(n=39) 5/39 (13%) Multicenter, prospective, randomized, single-blind study comparing the efficacy and gastrointestin al complications of early jejunal feeding with early gastric feeding Crit Care in critically ill Montejo JC, Grau Med 2002, patients. T, Acosta J, et al. 30:796-800 SB(n=50) 19/50 (38%) APACHE2=18( mean) 5日を越えて 栄養療法が必 要な症例 N=101 Gastric(n=51) 22/51 (43%) Gastric versus smallbowel tube feeding in the intensive care unit: a prospective comparison of Neumann DA, efficacy. DeLegge MH 1/35 (3%) 16/50 (32%) 20/51 (39%) 10.4 ± 1.2 平均±SD 15 ± 10 18 ± 16 23.0 ± 3.4 h 第7日目での栄養充足率 エネルギー投与量(mean) (mean) 消化管出血 0/35 (0) 下痢 3/35 (9) 1286 ± 344 下痢 7/50 (14%) 嘔吐 4/50 (8%) 75% ± 30% 1237 ± 342 下痢 7/51 (14%) 嘔吐 2/51 (4%) 栄養投与を行おう とし始めた時間か ら投与開始までの 時間 栄養チューブ挿 入開始から目標 投与量までの到 達時間 80% ± 28% C.Random: not sure ITT: yes Blinding: no 栄養チューブ 挿入完了から 目標投与速度 到達までの時 間 Crit Care Med 2002, 30:1436-1438 MICU (n = 60) Post pyloric (n =NR 30) 成人重症症例 、 5日を越え て栄養療法が 必要な症例 Mean APACHE II score: NR NG (n = 30) NR 27.0 ± 22.6 43.0 ± 24.1 h 17.3 ± 15.7 誤嚥 1/30 (3%) 11.2 ± 11.0 28.8 ± 15.9 h 17.0 ± 11.9 誤嚥 0/30 (0%) For Puclic Comment 表2B-1. 4ページ C.Random: not sure ITT: yes Blinding: no Gastric vs small-bowel feeding in critically ill children receiving mechanical ventilation: a randomized controlled trial. Meert KL, Daphtary KM, Chest Metheny NA. et al 2004;126:872 ICU患者にお ける幽門後栄 養チューブの 使用経験につ いて―医療リ 野口 佳奈, 河田 スクを減らす 玲奈, 安田 健司 ために et al Pediatric, mixed, postpyloric ventilated (PRISM score 8.2) 脳血管障害症 例30例、 JJPEN 2005 20 51APACHE2:NA ED(n=15) 11.1+-2.1 NG(n=15) NR 誤嚥 嘔吐 エネルギー充足率 20/30(67%) 19/32(59%) 10/30(33%) 10/32(31%) 47+-22% 30+-23% NR pseudo ramdamization OPEN label, 1ICU 逆流、嘔吐:な し、腹部膨 満:4/15(27%) 逆流、嘔 吐:3/15(20%), 腹部膨満:な し 10.2+-2.7 Canadian, SCCMでは不 採用 A randomized study of early nasogastric versus nasojejunal feeding insevere Eatock FC, Chong acute P, Menezes N et pancreatitis. al. Am J Gastroenterol 2005, 100:432439 Adult patients with severe acute pancreatitisMe dian age: 60 yearsMale: 53%Median APACHE II score at day1: 11Mechanicall y ventilated patients: 15 (31%) Patients admitted to ICU: 15 (31%) NJ (n = 22) NG (n = 27) 50%未満の症 例しかICUに は行っていな い 7/22(31.8) 5/27(18.5) 下痢 Early enteral nutrition in severe acute pancreatitis: a prospective randomized controlled trial comparing nasojejunal and nasogastric Kumar A, Singh N, routes. Prakash S,et al. J Clin Gastroenterol 2006,40:431434. Adult patients with severe acute pancreatitis as defined by Atlanta criteriaAdmitt ed to ICU Mean age: 40 years Males: 83%Mean APACHE II score: 10Respiratory failure: 19 (63%) NJ(n=14) NG(n=16) 4/14(27%) 5/16(31.3%) 1/14(6.7%) 3/15(20%) 4/16(25%) 0 For Puclic Comment 表2B-1. 5ページ RCT 平均 Duodenal versus gastric feeding in medical intensive care unit patients: a prospective, Crit Care Med randomized, Hsu CW, Sun SF, 2009, 37:1866clinical study. Lin SL, et al. 1872. Medical ICU人 工呼吸症例。 3日を越えて 栄養療法が必 要な症例 NJ(n=59) N=121 A randomised controlled comparison of early postpyloric versus early gastric feeding to meet nutritional targets in ventilated White H, intensive care Sosnowski K, patients. Tran K, Medical ICU 人工呼吸を行 う症例 APACHE2=27( Crit Care 2009, mean),群間で 13: APACHE2は R187. 有意差有り NJ(n=50) N=108 Gastric versus transpyloric feeding in severe traumatic brain injury: a prospective, randomized trial. NG(n=62) NG(n=54) 頭部外傷にて ICUで48時間 以上人工呼吸 Acosta-Escribano をおこなう症 J, FernandezIntensive Care 例、 Vivas M, Grau Med 2010, APACHE2=17( Carmona T, 36:1532-1539. mean) NJ(n=50) N=104 NG(n=54) 26/59 (44%) 24/62 (39%) 11/50 (22%) 5/54 (9%) 6/50 (12%) 9/54(16.7%) 5/59 (9%) 15/62 (24%) 5/50 (10%) 11/54 (20%) 16/50 (32%) 31/54 (57%) 平均 平均 栄養充足率 (mean)エネルギー投与量蛋白投与量 (kcal/day) (grams/day) 28.5 ± 24.9 18.20 ± 11.20 31.7 + 21.1 中央値(範囲)および平均,SD 嘔吐 8/62 (13) 消化管出血 9/62 (15) 目標到達まで の時間 23.8 ± 18.2 83 ± 6 1426 ±110 58.8 (4.9) 54.5 hrs 中央値(範囲)および平均,SD エネルギー投与量(中央値、四分位点) 蛋白投与量(中央値、四分位点) 目標までの到達時間 5.3 (2.73-9.89) 7.12 ± 6.00 (51) 3.93 (2.3-8.38) 5.73 ± 5.29 (51) 1463 (1232-1804) 63 (50-78) 5.02 (1.989.99) 9.10 ± 10.55 (55) 平均,SD 平均,SD 3.92 (1.5-8.54) 7.68 ± 9.81 (55) 1588 (913-1832) 69 (45-87) 平均,SD エネルギー充足率 (mean,SD) 18 ± 7 (54) 38 ± 24 (50) 7.3 ± 4 (50) 41 ± 28 (54) 8.9 ± 4 (54) 92 ± 7 84 ± 15 For Puclic Comment 表2B-1. 6ページ 1658 ± 118 67.9 (4.9) C.Random: Yes ITT: Yes Blinding: No (9) 18.20 ± 11.80 36.0 ± 24.2 16 ± 9 (50) 95 ± 5 嘔吐 1/59 (2%) 消化管出血 7/59 (12%) 目標到達まで の時間 32.4 hrs 4.1 (3.4-5.0) hrs C.Random: Yes ITT: Yes Blinding: No 4.3 (4.0-5.0) GIT C.Random: No complications ITT: Yes 7/50 (14) Blinding:no GIT complications 27/54 (47) 中央値(範囲) 中央値(範囲) 中央値(範囲) および平 および平 および平 エネルギー充足 均,SD 均,SD 均,SD 率 (mean, SD) A multicenter, randomized controlled trial comparing early nasojejunal with nasogastric Davies AR, nutrition in Morrison SS, critical illness. Bailey MJ Crit Care Med 2012, 40:23422348. 重症患者で人 工呼吸を受 け、鎮静薬を 投与されてい る、16歳以上 の症例。 APACHE2=20( mean) N=181 NJ(n=91) NG(n=89) Severity of illness influences the efficacy of enteral feeding route on clinical outcomes in J Acad Nutr patients with Huang HH, Chang Diet 2012, critical illness. SJ, Hsu CW et al. 112:1138-46 medical ICU, 24時間以上人 工呼吸を必要 とする症例 Mean APACHE II score: 21 n=101 ND (n = 50) NG (n = 51) Evaluation of early enteral feeding through nasogastric and nasojejunal tube in severe acute pancreatitis: a noninferiority randomized Singh N, Sharma controlled B, Sharma M, et trial. al. 13/91 (14%) 18/91 (20%) 12/89(13%) 19/89 (21%) 10 (7-15) 12.5 ± 8.6 20 (11-33) 28.8 ± 26.1 8 (6-12) 9.8 ± 6.2 11 (7-16) 12.7 ± 9.8 mean(SD) 24 (15-32) 27.4 ± 21.1 8 (5-14) 9.7 ± 6.3 72 % エネルギー投与 量 1497 ± 521 71% 1444 ± 485 エネルギー充足率 (mean, SD) 合併症 出血 2/91 (2%) 少量の出血 12/91 (13) 嘔吐 30/91 (33%) 誤嚥 5/91 (5%)下痢 26/91 (29%) 腹部膨満 16/91 (18%) 出血 2/89 (2%) 少量出血 3/89 (3%) 嘔吐 30/89 (30%) 誤嚥 4/89 (5%) 下痢 26/89 (30%) 腹部膨満 18/89 (20%) C.Random: Yes ITT: Yes Blinding: No 出血 7/50 (15%) 20/48(41.7%) 17/48(35.4%) 5/50(10%) 9/51(17.6%) 17.2(11.4) 50(16.9) 90.4 +/- 20.5% 76.2 +/- 24.9% Random: Yes Hsuのデータと 同じものを 使っているた め、メタアナリ シスには使用 できないため Canadianでは 外されている 出血 8/51 (15.7%) Pancreas 2012, NJ (n = 39) 41:153-159. Adult patients with severe acute 7/39(18) pancreatitisas defined by:Atlanta criteria, APACHE II > 8 or CT severityindex NA> 7All patients were admitted to ICU.Mean 感染症発生 age: 39 yearsMales: 35.90% 68%Median RCT APACHE II score: 8.2 NG (n = 39) 4/39(10.3) 23.10% Endoscopic placement 有意でない 有意 For Puclic Comment 表2B-1. 7ページ NTT=8.胃か ら投与すると 感染症発生が 抑えられる。 (非劣勢試験) Blinding: No comparison of nose jejunal tube and nasogastric tube in providing early enteral nutrition for patients with severe craniocerebral Zeng R-c, Jiang injury. F-g, Xie Q: Can percutaneous endoscopic jejunostomy prevent gastroesophag eal reflux in patients with preexisting Lien HC, Chang esophagitis CS, Chen GH. 詳細不明 不採用:詳細 不明。本文も 手に入れられ ず。 % Time esophageal pH <4 不採用:詳細 不明。本文も 手に入れられ ず。 Chinese J Clin Nutr Adult 2010, patients 18:3. with NJ (n severe = 20) craniocerebralinjuryMean age: 40 yearsMales: 63%Mean APACHE II score: NR NG (n = 20) Am J Gastroenterol. Neuro 2000 CVA ;95:3439-43. (n = 8) 経皮的挿入です。 12.9 min (4.9-28.2) 24.0 min (19.0-40.6) For Puclic Comment 表2B-1. 8ページ Blinding: no 経皮的挿入で ある。
© Copyright 2024